Connect With Us
Blog

Treatment and Prevention of Athlete’s Foot
 Athlete's foot, or tinea pedis, is a common fungal infection affecting the skin on the feet. It typically causes a red, itchy, and scaly rash, often starting between the toes. The condition thrives in warm, moist environments, making locker rooms, swimming pools, and communal showers common places for contraction. Athlete's foot occurs when the fungus comes into contact with the skin and finds favorable conditions to grow, such as damp socks or shoes. Symptoms include itching, burning, peeling skin, and in severe cases, blisters or ulcers. For mild cases of athlete's foot, antifungal creams, powders, or sprays may be effective. Keeping feet clean and dry is essential, as is changing socks regularly and wearing breathable footwear. Preventative measures include using shower sandals in public areas, thoroughly drying feet after washing, and avoiding sharing towels or shoes. If symptoms of athlete's foot persist or worsen despite treatment, it is suggested that you schedule an appointment with a podiatrist.
Athlete's foot, or tinea pedis, is a common fungal infection affecting the skin on the feet. It typically causes a red, itchy, and scaly rash, often starting between the toes. The condition thrives in warm, moist environments, making locker rooms, swimming pools, and communal showers common places for contraction. Athlete's foot occurs when the fungus comes into contact with the skin and finds favorable conditions to grow, such as damp socks or shoes. Symptoms include itching, burning, peeling skin, and in severe cases, blisters or ulcers. For mild cases of athlete's foot, antifungal creams, powders, or sprays may be effective. Keeping feet clean and dry is essential, as is changing socks regularly and wearing breathable footwear. Preventative measures include using shower sandals in public areas, thoroughly drying feet after washing, and avoiding sharing towels or shoes. If symptoms of athlete's foot persist or worsen despite treatment, it is suggested that you schedule an appointment with a podiatrist.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact one of our podiatrists from Brondon Foot and Ankle. Our doctors will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our office located in Centerville, OH . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Athlete’s Foot
Athlete’s foot, or tinea pedis, is a skin disease caused by a fungal infection. The infection typically occurs between the toes, and the feet are most subject to this disease because shoes best create the warm, dark, and moist environment in which fungus thrives. Other areas that create a similar environment, such as swimming pools, public showers, and locker rooms; can also promote fungi growth.
Symptoms of athlete’s foot include dry skin, itching, scaling, inflammation, and blistering. Sometimes, blisters can evolve into the cracks or breaks in the skin. The exposed tissue can then create pain, swelling, and discharge. The spread of infection can cause itching and burning as well.
While athlete’s foot commonly occurs between the toes, it may also spread to the toenails or soles of the feet. Other parts of the body, such as the groin or underarms, can also become infected if they are touched after the original area of infection is scratched. Aside from physical contact, athlete’s foot can also spread through the contamination of footwear, clothing or bedsheets.
Proper foot hygiene is essential in preventing athlete’s foot. You can prevent the fungus from spreading by frequently washing your feet using soap and water, thoroughly drying the feet between the toes, changing shoes and socks every day to reduce moisture, and ensuring that bathroom and shower floors are disinfected. Other tips include using shower shoes, avoiding walking barefoot in public environments, wearing light and airy shoes, and wearing socks that keep the feet dry.
While treatment for athlete’s foot can involve topical or oral antifungal drugs, mild cases of the infection can be treated by dusting foot powder in shoes and socks. Any treatment used can be supplemented by frequently bathing the feet and drying the toes. If proper foot hygiene and self-care do not ease your case of athlete’s foot, contact your podiatrist. He will determine if the underlying cause of your condition is truly a fungus. If that is the case, a comprehensive treatment plan may be suggested with the inclusion of prescription antifungal medications.
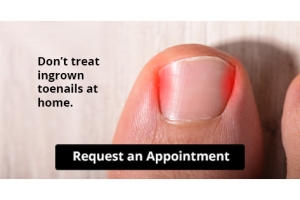
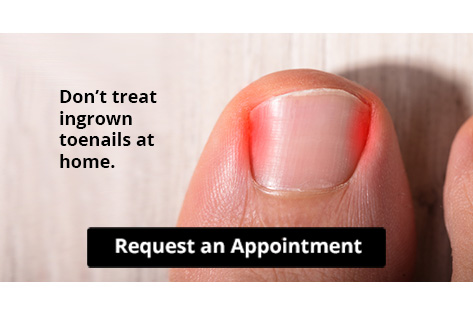
Let the Expert Treat Your Ingrown Toenails
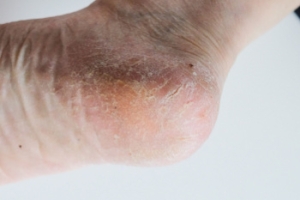
Causes of Cracked Heels
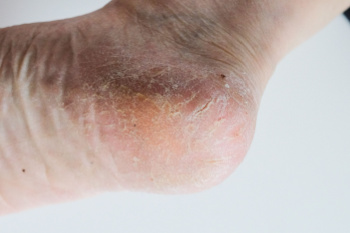
Cracked heels can result from various factors, including dietary deficiencies. Insufficient intake of essential vitamins like A, C, and E, as well as minerals such as zinc and iron, can contribute to dry, flaky skin prone to cracking. A diet lacking in omega-3 fatty acids may also impair skin hydration and elasticity, causing heel fissures. Additionally, dehydration plays a critical role, as inadequate water intake reduces skin moisture, making heels more susceptible to cracking. Other causes include prolonged standing or walking barefoot, which increases pressure on the heels, and wearing open-back shoes that fail to support the heel adequately. Cracked heels can be painful and unsightly. If you have developed this condition, it is suggested that you consult a podiatrist who can provide effective treatment solutions, which often includes prescribed medication.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact one of our podiatrists from Brondon Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in Centerville, OH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels may make you want to think twice about showing off your feet in warmer weather. However, cracked heels may be harmful to more than just the appearance of your feet. If deep fissures and cracks develop in your heels, they may make walking and standing painful for you. Additionally, these openings make way for germs to enter through your skin and cause infection.
There are several different causes of cracked heels. One of the most common reasons for this ailment is dry skin. This problem may make your keeps feel rough tight and itchy. Dry skin may be caused by cold air, extremely hot water, harsh soaps, and aging. Skin disorders such as eczema and psoriasis may eventually lead to dry skin. In some cases, complications may arise from cracked heels. Some of these complications are a loss of feeling in the heel, cellulitis, or a diabetic foot ulcer.
There are ways you can try to prevent getting cracked heels. One of the best ways to do so is to avoid wearing flip flops and sandals because these shoes increase your risk of drying out your feet. You should also avoid wearing shoes with a tall skinny heel, because these shoes cause your heel to expand sideways. At night, you should slather on a thick moisturizing cream on your feet and then cover them in socks to keep your feet moisturized overnight. Drinking water to stay hydrated is also a good way to ensure that your skin doesn’t become dry.
If you suffer from a severe case of cracked feet, you should make an appointment with your podiatrist to see what treatment methods are best for you.
How Serious Is My Heel Pain?

Heel pain can be debilitating, affecting daily activities and mobility. Common causes include plantar fasciitis, Achilles tendonitis, and heel spurs. Symptoms often manifest as sharp or dull pain in the heel or underside of the foot, especially noticeable after periods of rest. Effective treatment strategies include exercises to alleviate discomfort and reduce inflammation. Wearing proper footwear with adequate support and cushioning can also provide relief. Accurate diagnosis by a podiatrist is key for targeted treatment plans. So, if heel pain persists or worsens over time, it is wise to seek professional advice from a podiatrist. Their specialized knowledge ensures you receive comprehensive care and personalized treatment to address the root cause of your discomfort effectively. Don't let heel pain sideline you, and consider scheduling an appointment with a podiatrist for expert guidance and relief.
Many people suffer from bouts of heel pain. For more information, contact one of our podiatrists of Brondon Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Centerville, OH . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Have you ever gotten up from a chair or out of bed in the morning, and upon taking that first step, feel like your heel has stepped on a tack? Many people experience a feeling of sharp pain which radiates into their arch from their heel and which does not allow them to put their heel on the floor. Sometimes they need to sit back down, stand only on their toes and use the wall for balance. If you can take a few steps, it seems to go away and lessen, allowing you to then resume your activity. Later, throughout your day and after a period of rest, it can happen again. If this sounds familiar you may be suffering from your first attack of heel pain.
Heel pain is a debilitating condition that affects day to day activities. Running and walking both causes stress on the heel because the heel is the part of the foot that hits the ground first. This means that the heel is taking on your entire weight. Diagnosis and treatments for heel pain can be easily found through your podiatrist.
Plantar Fasciitis
One of the main causes of heel pain is a condition known as plantar fasciitis. The plantar fascia is a band of tissue that extends along the bottom of the foot, from the toe to the bottom of the heel. A rip or tear in this ligament can cause inflammation of these tissues, resulting in heel pain. People who do not wear proper fitting shoes are often at risk of developing problems such as plantar fasciitis. Unnecessary stress from ill-fitting shoes, weight change, excessive running, and wearing non-supportive shoes on hard surfaces are all causes of plantar fasciitis.
Achilles Tendonitis
Achilles tendonitis is another cause of heel pain. Similar to plantar fasciitis, inflammation of the Achilles tendon will cause heel pain due to stress fractures and muscle tearing. A lack of flexibility of the ankle and heel is an indicator of Achilles tendonitis. If left untreated, this condition can lead to plantar fasciitis and cause even more pain on your heel.
Heel Spur
A third cause of heel pain is a heel spur. A heel spur occurs when the tissues of the plantar fascia undergo a great deal of stress, leading to a separation of the ligament from the heel bone entirely. This results in a pointed fragment of bone on the ball of the foot, known as a heel spur.
Recognizing Common Symptoms of a Broken Foot

A broken foot can present with several clear symptoms, and it is vital to identify them for prompt treatment. One of the most telling signs is a sharp, severe pain that often worsens with movement or weight-bearing activities. A sensation of dislocated bones, where the foot feels misaligned or abnormal, is also common. Swelling and bruising typically develop rapidly around the affected area, indicating internal bleeding and inflammation. Visible deformities or an inability to move the foot or toes may also occur, in addition to a pronounced tenderness when touching the injured area. Treatment may include immobilization with a cast, use of crutches, and in severe cases, surgical intervention to realign the broken bones. If you feel you may have broken your foot, it is suggested that you consult a podiatrist who can accurately diagnose it and treat it accordingly.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact one of our podiatrists from Brondon Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in Centerville, OH . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment for a Broken Foot
The human foot has 26 different bones, and the foot is divided into three parts: the hindfoot, the midfoot, and the forefoot. Each section of the foot is composed of a different amount of bones. For instance, the forefoot is made up of 19 bones. The midfoot is composed of five smaller bones called the navicular, cuboid, and three cuneiform bones. Lastly, the hindfoot is made up of only the talus and the calcaneus. The feet tend to be vulnerable to slipping and twisting; consequently, fractured bones within the foot are common. When a bone gets crushed, bent, twisted, or stretched it may become broken.
Many foot fractures occur through an accident or trauma. More specifically, common causes for broken feet are car accidents, falls, missteps, or overuse. If you have a broken ankle or foot, you may have one or more of the following symptoms: throbbing pain, swelling, bruising, tenderness, deformities, and difficulty walking.
There are some factors that may put you at a higher risk of developing a broken foot. People who participate in high-impact sports are more likely to develop foot fractures because of the stresses, direct blows, and twisting injuries involved in gameplay. Additionally, those who suddenly increase their activity level are more likely to suffer a stress fracture.
Unfortunately, there are different complications that may arise because of a foot fracture. For instance, arthritis may be caused by fractures that extend into the joints. Bone infections are also possible in open fractures due to the bone being exposed to bacteria. However, there are ways you can help prevent yourself from breaking your foot. One way to avoid fractures is to wear proper footwear. If you plan on going on a run, you should wear running shoes. You should also replace your shoes if you notice that they are becoming worn out. For runners, it is best to replace shoes every 300 to 400 miles.
Treatment for foot fractures usually consists of rest, ice, elevation, and compression (RICE). If you plan on wrapping your foot, try not to wrap it too tightly because doing so may cut off blood supply in the foot. You should also avoid walking on the fractured foot.
If you suspect you have a broken foot, you should see your podiatrist right away. It is important that you have someone bring you to your doctor, since driving with a broken foot can be dangerous. You should especially seek urgent care if you are experiencing numbness, pain, or deformities in your foot.
Pronation Can Affect Your Running

Pronation is the natural side-to-side movement of the foot during walking or running. It is essential for shock absorption and navigating uneven surfaces. However, problems arise when this movement is excessive. Overpronation, where the foot rolls too far inward, can cause prolonged ground contact and increased stress on the leg's alignment. This may lead to injuries like plantar fasciitis, shin splints, and knee pain. Conversely, underpronation, or insufficient inward roll, causes the foot to remain rigid, failing to absorb shock effectively. This places undue stress on the outer edge of the foot, increasing the likelihood of stress fractures. Identifying pronation issues can often be done through a professional gait analysis conducted by a podiatrist. In some cases, a podiatrist might recommend custom orthotics to provide additional support and correct alignment issues. Selecting appropriate footwear and strengthening foot and ankle muscles can help manage pronation-related problems. If you experience foot pain linked to pronation, it is suggested that you make an appointment with a podiatrist for an exam and treatment.
If you have any concerns about your feet, contact one of our podiatrists from Brondon Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our office located in Centerville, OH . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.